
Image from people’s pharmacy via Google images
Alopecia refers to hair loss. Depending on whether the hair follicle is completely damaged or not, it is divided into scarring and non scarring alopecia. In scarring alopecia, the hair follicle has undergone fibrosis and is replaced by scar tissue. In non scarring alopecia, there is no fibrosis of the hair follicle.
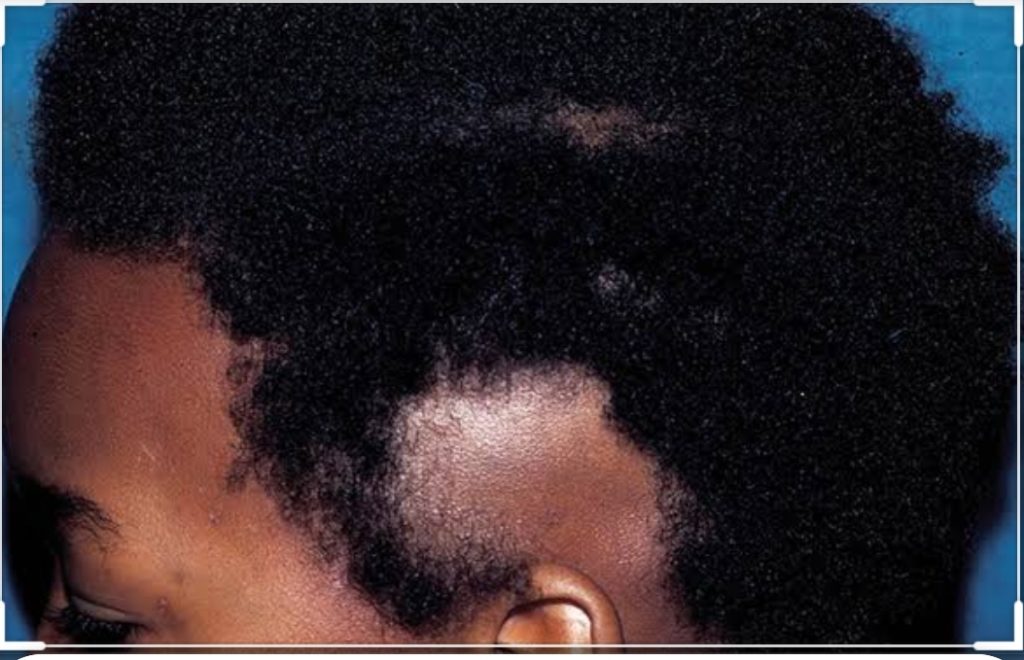
Alopecia areata is a type of non scarring alopecia that the cause is not completely clear. Studies have however shown that it is likely a T cell mediated autoimmune condition in a genetically susceptible individual. Remember I’ve said it before that autoimmune conditions are those in which the body no longer recognizes it’s own self and is fighting against ‘itself’.
Several diseases have autoimmunity as a basis for the cause. One of the evidence supporting alopecia areata as an autoimmune disease is that it tends to cluster with other autoimmune diseases like autoimmune thyroid disease, pernicious anaemia, vitiligo, diabetes mellitus, rheumatoid arthritis amongst others. I’ve had a patient with vitiligo, alopecia areata and Hashimoto’s thyroiditis before.
It can occur at any age but appears to be more common in the 2nd to 3rd decade of life. The Male:Female ratio is almost equal.
Alopecia areata can affect any hair bearing part of the body; the most commonly affected area is the scalp. Other areas like the beard, the armpits, eyebrow, groin…any other hair bearing area can be affected. The most common presentation is a single patch of hair loss without any symptoms. Some people may complain of itching in the area. Usually no scaling is seen.
There may be hair loss in several areas of the scalp in patches. There are different patterns of involvement on the scalp. If it affects the sides and back (like temporal and occipital) but spares the center, that’s called the ‘ophiasis’ pattern. If it spares the affects the centre majorly but spares the sides, that’s called the ‘sisaipho’ pattern.
If you have total involvement of all the hair on the scalp without any other area, that’s called alopecia totalis. If it affects all hair bearing areas including the scalp, that’s called alopecia universalis.
This is important to note for counseling as the prognosis is not as favorable in the ophiasis, totalis and universalis pattern.
There may also be nail changes as shown in the picture. The most common nail abnormality is nail pitting. May be seen in as high as 60% of patients. Other changes include Beau’s lines, leukonychia, brittle nails amongst others.
How do you manage? It is very important to counsel the patient/caregiver. Some may not respond to treatment especially those ones that have a poor prognosis ab initio. It is important to note that hair regrowth can occur on it’s own even without treatment. Some of the treatment used include topical and intralesional steroids, immunosuppressive medications amongst others. Camouflage is also an option for areas like eyebrow and scalp.
Counsel your patients adequately and let them read more on patient friendly sites like healthline. The condition has a lot of emotional and psychological impact.
Can you mention three other conditions where you can find nail pitting?
Can you mention two other causes of non scarring alopecia?
Pictures from American Family Physician and Pinterest via Google images.
So that’s it….Any comments, questions or clarifications? Image from Indiamart
Image from Indiamart


